As a new Alzheimer’s treatment awaits approval, the Alzheimer’s Association has released its updated diagnostic criteria, emphasizing the use of biomarkers like beta amyloid and tau proteins detected through lab tests or brain scans. This marks a significant shift from traditional pen-and-paper memory and thinking assessments in disease diagnosis.
The rationale behind these changes, according to the authors, is to detect Alzheimer’s in its earliest and potentially more treatable phases, possibly before symptoms manifest. However, this approach also raises concerns that individuals could receive an Alzheimer’s diagnosis based solely on a blood test, regardless of whether they exhibit memory impairments.
The authors advocate for a biological basis for diagnosis, emphasizing that symptoms alone should not determine Alzheimer’s diagnosis. They argue that individuals without current symptoms could still develop them in the future.
However, critics, including external experts and drug industry watchdog groups, argue that beta amyloid proteins can be present in the brain and blood without leading to dementia symptoms. They also highlight the lack of evidence supporting the efficacy of costly and potentially risky injected medications administered before symptom onset for long-term benefits.
Balancing the Pros and Cons of Early Diagnosis
In clinical trials, the new drugs — antibodies targeting beta amyloid to clear brain plaques — demonstrated moderate benefits. Beta amyloid peptides are protein fragments that accumulate into sticky brain plaques, often alongside tau protein, which forms tangles disrupting nerve cell communication, both hallmarks of Alzheimer’s disease.
Debate Continues Over Beta Amyloid’s Role in Alzheimer’s Disease, Some Experts Suggest Plaques Are a Result Rather Than a Cause
In an 18-month study involving individuals in the early stages of Alzheimer’s disease, the FDA-approved antibody lecanemab slowed cognitive decline by 27% compared to a placebo. Similarly, the experimental drug donanemab showed a 35% reduction in disease progression compared to placebo last year, leading an FDA advisory group to recommend its approval for Alzheimer’s treatment. However, these drugs carry risks such as brain fluid accumulation, swelling, and microbleeds, which may necessitate hospitalization. Studies have not shown benefits from antibody treatments in patients with amyloid buildup but no symptoms.
There is no scientific evidence to support it,” stated Dr. George Perry, a neurobiologist and editor of the Journal of Alzheimer’s Disease.
Critics argue that the new criteria could significantly increase the pool of eligible candidates for new drugs, potentially resulting in substantial profits for drug manufacturers.
“The Alzheimer’s Association risks credibility by endorsing guidelines that classify perfectly healthy individuals as having Alzheimer’s disease,” remarked Dr. Adriane Fugh-Berman, director of PharmedOut, a Georgetown University program that monitors pharmaceutical marketing strategies.
If followed, these guidelines will ruin the lives of tens of thousands of people who will be misinformed that they have dementia,” she said. “The only entities that gain from this travesty are the pharmaceutical companies that make drugs for Alzheimer’s and the Alzheimer’s Association, which is preying on fear.”
The Alzheimer’s Association says its criteria is based on the latest developments in Alzheimer’s science. Because Alzheimer’s therapies haven’t been approved for people without symptoms, for now, it recommends against diagnostic testing in people without cognitive impairment, according to the working group that developed the criteria.
“Our goal in sharing them now — even as the field and our knowledge continues to evolve — is to advance diagnosis, treatment and prevention in order to improve individual care and reduce the societal impact of Alzheimer’s,” said Dr. Maria C. Carrillo, the Alzheimer’s Association’s chief science officer and medical affairs lead, and senior author on the new criteria.
Conflicts of Interest Regarding Financial Matters
The new criteria, developed by a 20-member working group from the leading patient advocacy organization for Alzheimer’s, have drawn attention due to financial conflicts of interest among its members. A significant portion of the panel, including a third directly employed by pharmaceutical companies and another third receiving payments from pharmaceutical or testing companies, has financial ties to entities involved in marketing or developing new Alzheimer’s drugs. Additionally, two panel members were Alzheimer’s Association employees, an organization that also accepts funding from pharmaceutical companies. Only a small number of members declared no relevant conflicts of interest.
We should question the reliance on guidelines influenced by industry,” stated Dr. Eric Widera, a geriatrician at the University of California San Francisco, who authored a commentary in the Journal of the American Geriatrics Society on the new criteria.
Widera criticizes what he sees as a familiar pharmaceutical industry tactic: expanding the disease diagnosis to broaden the market for a drug. “This is diagnostic creep,” he emphasized.
He pointed to examples such as Abbott Labs’ “Is it low T?” campaign, which promoted a testosterone replacement product along with a more sensitive hormone test. Biogen’s “It’s Time We Know” campaign similarly raised awareness about mild cognitive impairment after the controversial FDA approval of its Alzheimer’s drug Aduhelm in 2021, which has since been withdrawn from the market.
Under the new criteria, Widera estimates that up to 1 in 10 healthy 50-year-olds could test positive for beta amyloid. While about 6 million Americans currently live with Alzheimer’s, projections suggest approximately 40 million could test positive for beta amyloid.
“These publications serve as part of a strategy aimed at maximizing sales of monoclonal antibodies,” remarked Dr. Karl Herrup, a neurobiology professor at the University of Pittsburgh School of Medicine.
Justifying Industry Participation in Guidelines Development
Dr. Clifford Jack, a brain imaging researcher at the Mayo Clinic, spearheaded the development of the new guidelines and expresses pride in the committee’s achievements.
I authored approximately 99% of the final document and have no conflicts of interest,” stated Dr. Clifford Jack.
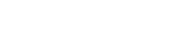
The authors attribute the guideline change to advancements in Alzheimer’s disease treatment and new blood tests for amyloid and tau proteins. These tests, available through specialized labs, await FDA approval pending rigorous validation to minimize false results.
In a commentary published in Nature Medicine, the work group emphasized its diverse composition, including members from industry, clinical medicine, academia, FDA, and the National Institute on Aging. They aimed to integrate varied perspectives to reflect the latest scientific knowledge.
“We aimed to incorporate the best current scientific insights, including industry research, which conducts these trials,” Jack remarked. “Throughout the process, there was no effort by any committee member to promote commercial interests in these guidelines.
The initial draft of the criteria, introduced at the Alzheimer’s Association International Conference in 2023, initially noted a collaboration between the Alzheimer’s Association and the National Institute on Aging. However, after facing criticism, the institute removed its name from the title following directives from the broader National Institutes of Health administration. This action was in adherence to an NIH policy against endorsing private entities, products, or services, as stated in an email from the National Institute on Aging.
The National Institute on Aging affirmed its continued participation in the working group and expressed its commitment to ongoing collaboration with the Alzheimer’s Association and other involved organizations.
Since the release of the draft criteria, the Alzheimer’s Association has clarified that they are not intended to serve as comprehensive diagnostic guidelines for clinicians. Instead, the criteria are positioned as a ‘bridge’ between research findings and clinical practice.
Development of Updated Guidelines Underway
The Alzheimer’s Association intends to assemble a fresh workgroup comprising different members to craft practical guidelines for diagnosing Alzheimer’s disease in clinical settings. The extent to which these guidelines will align with the diagnostic criteria remains uncertain.
According to Dr. Clifford Jack, the guidelines are expected to provide specific, actionable recommendations that may include references to particular commercial products.
Spokesperson Niles Franz affirmed the Alzheimer’s Association’s commitment to developing credible clinical practice guidelines and evidence-based recommendations to guide clinical decision-making at various levels, from individual to population health.
Franz emphasized that trustworthy guidelines, as outlined by the National Academy of Medicine, necessitate collaboration between organizing bodies and panels of experts who have minimal intellectual and financial conflicts.
The Association has recently implemented stringent protocols for collecting disclosures of conflict of interest from panel nominees, evaluating these disclosures, selecting members, and managing conflicts throughout and after guideline development,” he stated.
Franz expressed the association’s aim to finalize the new clinical guidelines for publication by 2025.
In the interim, Widera and others stress that the decision to use amyloid-clearing drugs is highly personal and should involve close consultation with a physician.
“There is arguably more controversy surrounding these guidelines than the drugs themselves,” noted Widera.
Looking ahead, Widera hopes the Alzheimer’s Association will address the risks in future guidelines.
“If the definition of a disease is broadened, it’s crucial to outline the associated risks and harms,” he emphasized.