Health & Wellness
This Radio DJ Turned into the Tables to Lose 48 Kilos
Published
3 years agoon

JOSEPH BENJAMIN, 27, let a day radio job meld into silly evening objects at the club. He’d drink no matter cocktail he became as soon as handed, became “true associates with the Uber Eats drivers,” won weight, and “didn’t delight in my physique.” In 2021, after a pair of year of this, he seen his respiratory sounded delight in snoring. He took control of his time table and habits, misplaced 48 pounds, and is now respiratory neutral pretty. How he did it:
MAKE THE GYM YOUR ENERGY DRINK
Benjamin started with a time table revamp. He compelled himself to develop trusty into a morning person when he became as soon as switched to an early radio shift. He’s now no longer a coffee man, so he depends on a 6:00 a.m. F45 class—functional working against in a group setting—to amp up for the day. (He even creates the remixes for the classes.) “It additionally instilled some roughly powerful-wished awareness of my physique,” he says. Now he’s more careful about what he does to it.
CLOSE THE KITCHEN EARLY
He stops exciting spherical 6:00 a.m.—three hours earlier than he goes to bed. Leisurely-evening exciting, he found out, is linked to silly-morning sound asleep and all-day sluggishness. He didn’t swap his meals powerful (that you just can silent uncover him with a burger as soon as in a whereas), nonetheless as soon as he started exciting earlier, slicing the silly-evening snacking, and getting to bed on time most nights (because“I’ve gotta be an grownup the following day”), the weight got here off.
Extra From Men’s Correctly being

ASK BEFORE YOU DRINK
When Benjamin does evening time gigs, he’s realized to expose down the free alcohol. To lose weight, he determined to drink easiest as soon as per week. He credit ranking his gymnasium routine with serving to him rep the discipline to total it—that and the Gain No longer Disturb feature on his mobile phone to steer particular of silly-evening invites. If he needs to imbibe, he asks himself, “Is that this drink definitely worth the break to my physique?” Most often, the respond is no longer any.
A model of this text first and well-known appeared within the September 2023 exclaim of Men’s Correctly being.
Cori Ritchey, NASM-CPT is an Affiliate Correctly being & Correctly being Editor at Men’s Correctly being and a licensed private trainer and group fitness trainer. That you can even rep more of her work in HealthCentral, Livestrong, Self, and others.
You may like
Health
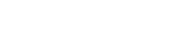
How to Get Featured in SF Weekly: A Complete Guide for Brands, Artists & Entrepreneurs
Published
2 hours agoon
February 24, 2026
Landing a feature in SF Weekly can dramatically boost your visibility, credibility, and reach in the Bay Area. Whether you’re a startup founder, artist, restaurant owner, or event organizer, getting featured in SF Weekly can open doors to new customers and media opportunities.
In this SEO-friendly guide, you’ll learn how to get featured in SF Weekly, step-by-step — plus insider tips to improve your chances of getting noticed.
Why Getting Featured in SF Weekly Matters

Before diving into the process, let’s understand why a feature is valuable:
-
Strong local credibility in San Francisco
-
Exposure to Bay Area readers and businesses
-
SEO benefits from authoritative backlinks
-
Increased brand trust and social proof
-
Media validation you can showcase in PR kits
If you’re targeting the San Francisco market, a feature in SF Weekly positions you as a serious local player.
How to Get Featured in SF Weekly (Step-by-Step)
1. Understand What SF Weekly Covers
To get featured in SF Weekly, you must align with their editorial focus. They typically cover:
-
Local news and culture
-
Arts & entertainment
-
Restaurants and food trends
-
Events and nightlife
-
Cannabis industry
-
Emerging businesses
-
Social impact stories
Pro Tip: Study recent articles and identify patterns in tone, story angles, and featured businesses.
2. Create a Newsworthy Angle
SF Weekly won’t feature you just because you ask. You need a compelling hook.
Ask yourself:
-
Are you launching something new?
-
Did you hit a major milestone?
-
Are you disrupting a local industry?
-
Is there a strong human-interest story behind your brand?
-
Are you hosting a unique San Francisco event?
Journalists want stories — not advertisements.
3. Build a Strong Media Kit
To increase your chances of getting featured in SF Weekly, prepare:
-
A professional bio
-
High-resolution photos
-
Brand story
-
Press releases (if available)
-
Social media links
-
Website link
-
Contact information
Make it easy for editors to cover you without extra work.
4. Find the Right Editor or Writer
Instead of sending a generic message, identify:
-
Editors covering your niche
-
Staff writers focused on your industry
-
Contributors who write similar stories
Then personalize your pitch.
Avoid:
Mass emails
Generic press releases without context
Overly promotional language
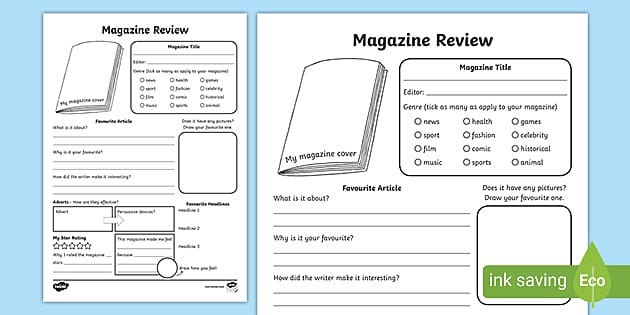
5. Write a Compelling Pitch Email
Here’s a simple pitch structure:
Subject Line: Story Idea: [Compelling Hook] in San Francisco
Email Body:
-
Short introduction (who you are)
-
Why your story matters to SF readers
-
Why it’s timely
-
Link to media kit
-
Offer availability for interview
Keep it under 200 words.
6. Leverage Local PR & Community Engagement
To improve your odds of getting featured in SF Weekly:
-
Attend San Francisco networking events
-
Collaborate with local influencers
-
Participate in community initiatives
-
Get involved in local charities
-
Build relationships with other featured businesses
Media attention often follows community visibility.
7. Use HARO & Media Platforms
Sign up for platforms where journalists request sources. Respond quickly and provide clear, concise insights.
Being proactive increases your visibility beyond just emailing editors directly.
8. Consider Sponsored Content (If Appropriate)
If your goal is guaranteed placement, explore advertising or sponsored editorial options directly through SF Weekly. This can be useful for:
-
Grand openings
-
Major product launches
-
Event promotions
Be transparent and choose the option that aligns with your brand strategy.
Common Mistakes to Avoid
If you want to successfully get featured in SF Weekly, avoid:
-
Pitching without researching the publication
-
Making the email too long
-
Sending low-quality photos
-
Following up excessively
-
Being overly sales-focused
Remember — editors are looking for stories that serve their audience.
How Long Does It Take to Get Featured?
There is no guaranteed timeline. It may take:
-
1–2 weeks for a response
-
1–3 months for publication
-
Multiple follow-ups before traction
Consistency is key.
Final Tips on How to Get Featured in SF Weekly
-
Build your personal brand online
-
Maintain active social media
-
Publish thought leadership content
-
Collect testimonials and press mentions
-
Stay relevant to San Francisco trends
Getting featured in SF Weekly isn’t about luck — it’s about strategy, positioning, and persistence.
Conclusion
If you’ve been wondering how to get featured in SF Weekly, the formula is simple:
-
Be newsworthy
-
Align with their audience
-
Pitch strategically
-
Build relationships
-
Stay consistent
Media coverage can transform your brand visibility in the Bay Area — and with the right approach, you can make it happen.
Health
Get Featured in Vanity Fair: The Ultimate Power Move for Your Personal Brand
Published
1 day agoon
February 23, 2026
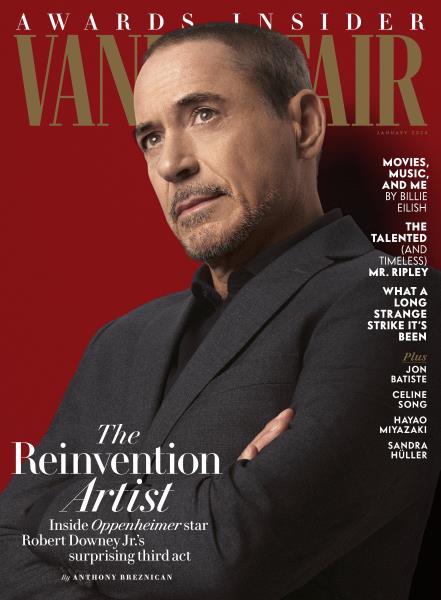


In the world of influence, credibility is currency. You can build a strong social media following, land podcast interviews, and even go viral — but there’s something different about seeing your name printed in the glossy pages of Vanity Fair.
It signals arrival.
For entrepreneurs, creatives, executives, and cultural tastemakers, being featured in Vanity Fair isn’t just a media win. It’s a brand-defining moment. It tells the world: You matter at the highest level.
In this edition of Level Up Magazine, we’re breaking down why Vanity Fair remains one of the most powerful platforms in media — and how positioning yourself for this kind of exposure can elevate your authority instantly.
Why Vanity Fair Still Holds Cultural Power
Founded in 1913 and reimagined for the modern era, Vanity Fair has long been a gatekeeper of influence. From Hollywood elites to political power players, the magazine doesn’t just report culture — it shapes it.
A feature in Vanity Fair means:
-
You’ve crossed into mainstream cultural relevance
-
Your story has narrative depth
-
Your influence extends beyond niche audiences
-
You’re perceived as premium
In today’s crowded digital landscape, perception is everything. Vanity Fair represents legacy media at its finest — highly curated, editorially selective, and globally respected.
While social media builds visibility, legacy publications build permanence.
What Vanity Fair Looks For
If you want to land on their radar, it’s important to understand what they value.
Vanity Fair is not interested in:
-
Generic success stories
-
Surface-level accomplishments
-
Trend-chasing personalities
They are interested in:
-
Cultural impact
-
Distinctive personal narratives
-
Power, influence, and transformation
-
Individuals shaping industries
Your story must feel larger than you.
Are you redefining leadership?
Disrupting an industry?
Challenging norms?
Creating movements?
Vanity Fair features people who represent shifts in culture — not just participants in it.
The Psychology of Being “Vanity Fair Worthy”
There’s a mindset shift required before the media recognition comes.
To be featured at that level, you must:
-
Think beyond local influence
-
Position yourself as a thought leader
-
Operate at premium standards
-
Curate your public image intentionally
Media is a mirror. It reflects how you already show up.
If your brand visuals are inconsistent, your messaging unclear, or your positioning too broad, you won’t attract high-level editorial attention.
Vanity Fair doesn’t create authority — it amplifies existing authority.
Building Toward the Feature
Getting featured in a major publication rarely happens randomly. It’s a result of strategic positioning.
Here’s the blueprint:
1. Elevate Your Narrative
Facts don’t get features — stories do.
Craft a compelling origin story:
-
What obstacles did you overcome?
-
What mission drives you?
-
What tension exists in your journey?
Editors look for depth, vulnerability, and relevance.
2. Strengthen Your Digital Footprint
When editors research you (and they will), what do they find?
-
Professional press photos
-
Clear brand identity
-
Media mentions
-
Thought leadership content
-
Strong website presence
Everything should align with a premium aesthetic.
3. Secure Stepping-Stone Media
Top-tier features often follow mid-tier exposure.
Think:
-
Industry publications
-
Podcasts
-
Authority blogs
-
Speaking engagements
Momentum builds credibility.
The Power of Association
When your name appears in Vanity Fair, you’re placed in proximity to cultural icons, global leaders, and entertainment royalty.
That proximity shifts perception instantly.
Suddenly:
-
Investors see you differently
-
Clients view you as elite
-
Collaborators approach you
-
Your speaking fees increase
Media credibility compounds.
And in high-level business, perception drives opportunity.
It’s Not Just About Fame — It’s About Positioning
Vanity Fair isn’t simply a celebrity magazine. It’s a publication that explores power — who has it, how they use it, and what it costs.
If you want to align yourself with that level of conversation, your brand must reflect:
-
Substance
-
Sophistication
-
Cultural awareness
-
Impact
This is about stepping into rooms where influence is exchanged at the highest level.
Becoming Feature-Ready
Ask yourself:
-
Does my story inspire beyond my industry?
-
Is my brand visually aligned with premium media?
-
Am I building cultural relevance — or just visibility?
-
Would a global audience find my journey compelling?
If not, that’s your next level.
Becoming “Vanity Fair ready” forces you to refine your message, elevate your standards, and think bigger about your impact.
Final Word: Think Legacy, Not Likes
In a world obsessed with algorithms, aim for legacy.
Being featured in Vanity Fair isn’t about ego — it’s about entering the historical record of influence. It’s about positioning your name alongside those shaping culture, business, art, and power.
At Level Up Magazine, we believe in building brands that don’t just trend — they endure.
The question isn’t whether you want to be featured.
The question is:
Are you building something worthy of it?
Level up accordingly.
Health
How to Get Featured in Daily Mail: A Strategic Guide for Brands and Experts
Published
4 days agoon
February 20, 2026
Being highlighted in a major publication can instantly elevate your credibility, visibility, and authority. One of the most influential platforms in global media is Daily Mail — a publication with millions of readers across the UK, the US, and beyond. If your goal is to get featured in Daily Mail, you need more than luck. You need strategy, timing, and a compelling story.
This guide walks you through the right approach to secure meaningful media coverage.
Why Media Coverage in a Major Publication Matters



A feature in a high-authority publication offers:
-
Massive exposure to millions of readers
-
Credibility boost for your brand or personal profile
-
SEO benefits from high-domain authority backlinks
-
Increased trust among customers and investors
-
Long-term brand positioning
Unlike paid ads, editorial coverage carries third-party validation — which makes it far more powerful.
Understand What Editors Are Looking For
Journalists and editors receive hundreds of pitches daily. To stand out, your story must align with what the publication values:
1. Strong News Angle
Is your story timely? Does it connect to trending topics, current events, or public interest discussions?
2. Human Interest
Personal journeys, unique challenges, and emotional stories often perform exceptionally well.
3. Data & Evidence
Research-backed insights, surveys, or original statistics increase credibility.
4. Celebrity or Influencer Connection
If your story involves a public figure, partnership, or social media traction, it becomes more attractive to editors.
Craft a Compelling Media Pitch
A strong pitch is concise, relevant, and tailored.
Key Elements:
-
Attention-grabbing subject line
-
Clear headline angle
-
2–3 short paragraphs explaining why the story matters
-
Supporting data or quotes
-
High-resolution images available upon request
Avoid generic mass emails. Personalize your pitch to the specific journalist who covers your niche.
Build Media Relationships
Media coverage rarely happens from a single cold email. Instead:
-
Follow journalists on social media
-
Engage thoughtfully with their articles
-
Provide value before asking for coverage
-
Become a reliable source in your industry
Long-term relationships significantly increase your chances of publication.
Leverage PR Professionals
If you have the budget, hiring a PR agency can accelerate the process. Experienced publicists:
-
Have established media contacts
-
Know how to position stories strategically
-
Understand editorial standards
-
Manage follow-ups professionally
A well-connected PR expert can bridge the gap between your story and the newsroom.
Create a Story That’s Bigger Than Promotion
One common mistake is pitching a product advertisement disguised as news. Instead of focusing on your business, frame the story around:
-
Industry trends
-
Social impact
-
Unique challenges you’ve overcome
-
Lessons others can learn
When your story serves readers first, editors are far more receptive.
Timing Is Everything
News cycles move quickly. Tie your pitch to:
-
Seasonal trends
-
Breaking news
-
Industry reports
-
Cultural conversations
Relevance increases urgency — and urgency increases coverage.
Optimize Your Online Presence
Before publishing, journalists often research sources. Make sure you have:
-
A professional website
-
Updated social media profiles
-
Clear bio and credentials
-
Press-ready photos
-
Prior media mentions (if available)
Credibility online supports credibility in print.
Final Thoughts
Securing coverage in a leading publication doesn’t happen by accident. It requires a strong narrative, strategic outreach, and persistence. Whether you’re an entrepreneur, expert, or brand, the key is positioning your story in a way that serves the audience first.
When you approach media with authenticity, relevance, and professionalism, your chances of gaining national — even global — attention increase dramatically.
If done correctly, that single feature can transform your visibility and open doors you never imagined.
Health
Get Featured in The New York Times: A Strategic Guide to National Media Recognition
Published
6 days agoon
February 18, 2026
In today’s competitive media landscape, credibility is everything. For entrepreneurs, founders, authors, and industry leaders, few achievements carry as much prestige as being featured in The New York Times. If you’re looking to Get Featured in The New York Times, you’re not just seeking publicity—you’re positioning your brand at the highest level of authority and influence.
But landing coverage in one of the world’s most respected publications requires more than luck. It demands strategy, storytelling, and strong media relationships.
In this guide, we’ll break down how you can strategically increase your chances of getting featured in The New York Times.
Why Getting Featured in The New York Times Matters
The New York Times isn’t just another media outlet. It’s a global publication read by millions of decision-makers, investors, journalists, and thought leaders.
Here’s what a feature can do for your brand:
-
Instant credibility and authority
-
Increased brand visibility nationwide and globally
-
Higher trust among clients and partners
-
Stronger investor confidence
-
Long-term SEO value and digital footprint
When your name appears in The New York Times, it becomes a powerful trust signal that sets you apart from competitors.
Step 1: Build a Newsworthy Story
Journalists at The New York Times don’t publish promotional content. They focus on stories that matter to their audience.
To increase your chances of getting featured, your story should be:
-
Timely and relevant
-
Data-driven or backed by strong evidence
-
Impactful at a local, national, or global level
-
Unique or disruptive within your industry
Ask yourself: Is this story interesting beyond my business? If the answer is yes, you’re on the right path.
Step 2: Develop a Strong Media Angle
Even great businesses don’t automatically qualify for media coverage. What makes the difference is the angle.
For example:
-
Did your company solve a major industry problem?
-
Are you pioneering a new trend?
-
Do you have compelling data that reveals something surprising?
-
Is your journey tied to a broader economic or cultural shift?
A powerful angle transforms a business milestone into a story journalists want to cover.
Step 3: Understand The Right Section
The New York Times has multiple sections including:
-
Business
-
Technology
-
Opinion
-
Lifestyle
-
Arts
-
Entrepreneurship
Research which section best aligns with your story. Sending a startup funding story to a lifestyle editor reduces your chances of success. Strategic targeting is critical.
Step 4: Craft a Professional Media Pitch
Your pitch should be concise, compelling, and journalist-focused.
A strong pitch includes:
-
A powerful subject line
-
A clear headline idea
-
Why the story matters now
-
Key statistics or proof points
-
Availability for interviews
Avoid making the pitch about you. Instead, frame it around the value for readers.
Step 5: Build Media Relationships
One of the most overlooked aspects of getting featured in The New York Times is relationship-building.
Journalists receive hundreds of pitches daily. Having established credibility and rapport significantly increases your visibility.
Ways to build relationships:
-
Engage with journalists on social platforms
-
Share their articles thoughtfully
-
Provide expert commentary when relevant
-
Respond quickly to media inquiries
Media exposure is rarely a one-time effort—it’s the result of consistent positioning.
Step 6: Strengthen Your Online Presence
Before publishing a feature, journalists often research your background.
Make sure you have:
-
A professional website
-
Clear messaging and brand positioning
-
Strong social media presence
-
Verified credentials and past achievements
Your digital footprint should reinforce your credibility.
Common Mistakes to Avoid
If you want to Get Featured in The New York Times, avoid these pitfalls:
-
Sending generic press releases
-
Overly promotional messaging
-
Lack of data or proof
-
Pitching without understanding the audience
-
Following up excessively
Precision and professionalism matter at this level.
The Role of Strategic PR Support
While it’s possible to pitch independently, working with experienced public relations professionals significantly improves your chances.
A strategic PR team can:
-
Identify the strongest story angle
-
Develop media-ready press materials
-
Connect with the right editors
-
Position you as an expert source
-
Manage follow-ups professionally
Media placements at the level of The New York Times require credibility, connections, and consistency.
Long-Term Benefits of Being Featured
Getting featured in The New York Times is more than a headline—it becomes a long-term brand asset.
You can leverage the coverage for:
-
Investor presentations
-
Website credibility sections
-
Social proof marketing
-
Speaking engagements
-
Partnership negotiations
A single feature can open doors for years to come.
Final Thoughts
To Get Featured in The New York Times, you must think like a journalist, not a marketer. Focus on delivering real value, strong data, and compelling storytelling. Build relationships, refine your positioning, and ensure your message aligns with what truly matters to readers.
Prestige media coverage doesn’t happen overnight—but with the right strategy, persistence, and professional execution, it becomes achievable.
If your goal is national credibility and global recognition, few platforms offer the impact of The New York Times. The key is approaching it with preparation, precision, and purpose.
Health
Why Every Founder Wants to Get Featured in TechCrunch
Published
1 week agoon
February 17, 2026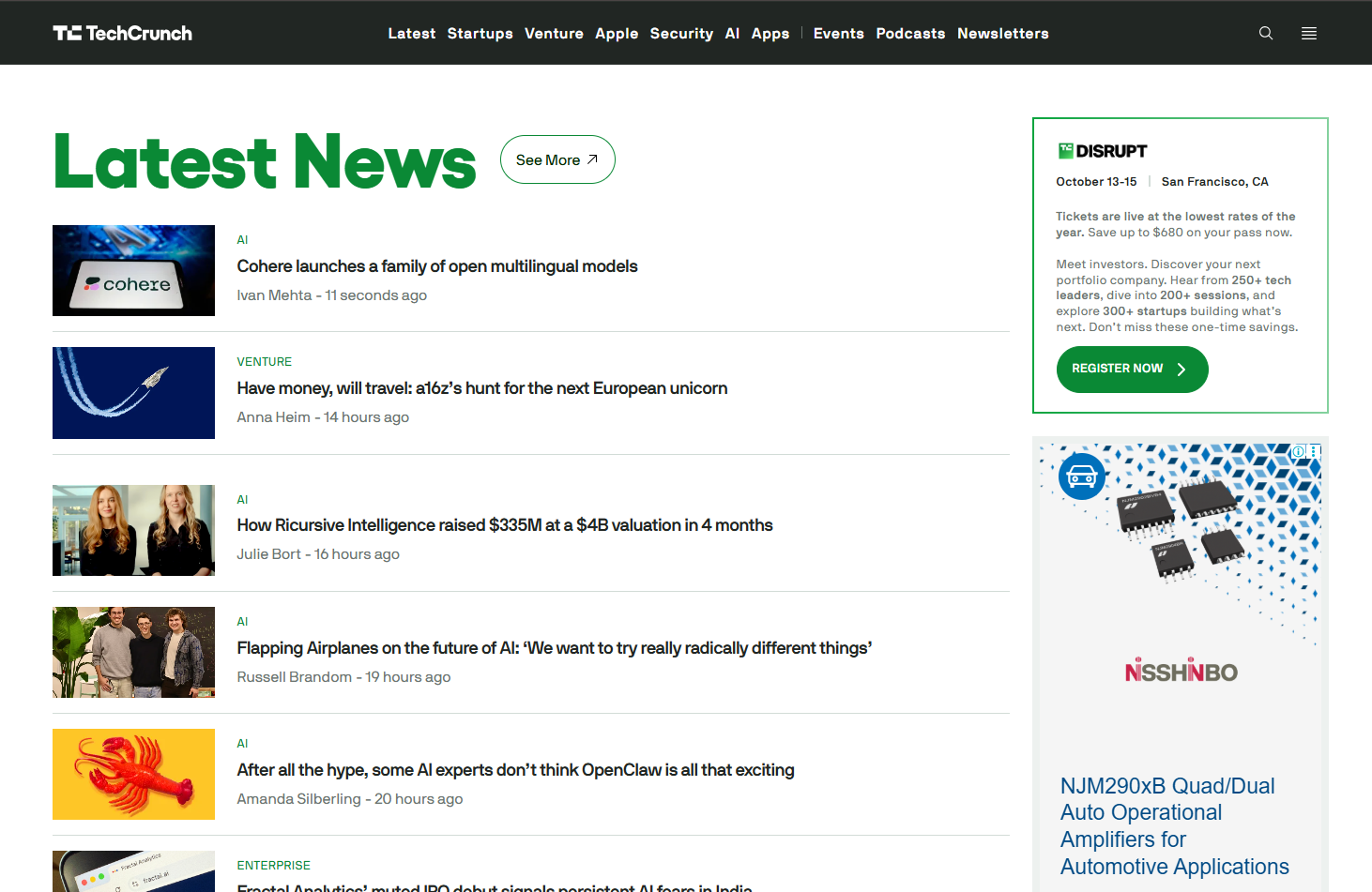
In the fast-paced world of startups and tech innovations, visibility can make or break your business. One of the most prestigious platforms for tech coverage is TechCrunch. Being featured in TechCrunch not only boosts your credibility but also opens doors to investors, potential customers, and media attention. In this guide, we’ll explore how to get featured in TechCrunch and make the most of this incredible opportunity.
Why You Should Aim to Get Featured in TechCrunch
Before diving into strategies, it’s essential to understand why being featured in TechCrunch is a game-changer. TechCrunch is recognized globally for covering emerging technologies, startup funding, and innovations. When your startup gets coverage here, it sends a strong signal to the industry that your business is worth noticing.
Some benefits of getting featured include:
-
Increased visibility: TechCrunch articles often go viral within the tech community, reaching thousands of readers.
-
Investor interest: Investors frequently scan TechCrunch for promising startups.
-
Enhanced credibility: Media coverage from a reputable source establishes trust with potential clients and partners.
Clearly, being featured in TechCrunch can accelerate your startup’s growth and reputation.
How to Prepare Your Startup to Get Featured in TechCrunch
Preparation is key when aiming to get featured in TechCrunch. Journalists are selective, and they tend to write about startups that have a compelling story, a unique product, and clear traction. Here’s how to prepare:
1. Perfect Your Story
TechCrunch loves stories, not just products. You should have a narrative that explains:
-
What problem does your startup solves
-
Why is your solution unique
-
How you’re disrupting the market
The story should resonate emotionally with readers. Startups that present a clear and engaging story often stand out.
2. Have Solid Metrics
TechCrunch journalists prefer startups with measurable progress. Whether it’s revenue growth, user adoption, or market expansion, having concrete metrics makes your story more compelling.
3. Create a Press Kit
A press kit helps journalists quickly understand your business. Include:
-
High-resolution logos and product images
-
Founder bios with professional photos
-
Key metrics and milestones
-
Previous media coverage (if any)
A well-prepared press kit makes it easier for journalists to cover your story and increases your chances to get featured in TechCrunch.
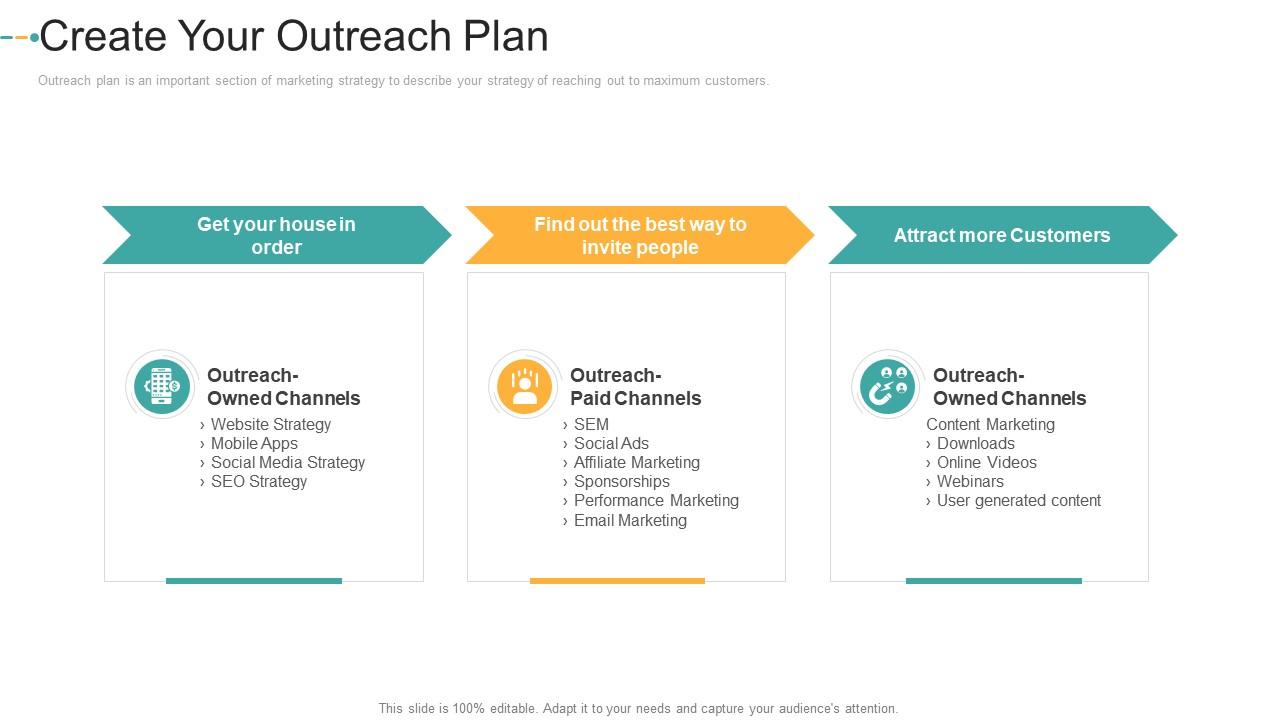
Strategies to Get Featured in TechCrunch
Once you’re prepared, it’s time to focus on strategies that can get your startup noticed by TechCrunch journalists.
1. Build Relationships with TechCrunch Journalists
Networking with journalists is crucial. Follow them on social media, comment on their articles, and understand what topics they cover. When you eventually pitch your story, it should feel personal and relevant to their interests.
2. Craft a Compelling Pitch
Your pitch email should be concise, engaging, and clearly outline why your story is newsworthy. Include your unique angle, key metrics, and why it matters to TechCrunch readers. Avoid sending generic press releases; personalization is critical.
3. Leverage Launch Platforms
Using platforms like Product Hunt or startup accelerators can create buzz that attracts journalists’ attention. A strong product launch with early user feedback increases your chances to get featured in TechCrunch.
4. Highlight Unique Angles
TechCrunch loves innovative, unusual, or disruptive stories. Think about what makes your startup different from competitors and emphasize that. For example, if your AI product is solving a problem in a novel way, make sure that’s the focus of your pitch.
Common Mistakes to Avoid
While trying to get featured in TechCrunch, startups often make mistakes that reduce their chances. Avoid these:
-
Overhyping your product: Exaggeration can backfire. Be truthful and transparent.
-
Ignoring journalist preferences: Not every story suits TechCrunch. Research before pitching.
-
Poor timing: Sending a pitch during busy news cycles can get your email lost.
Post-Feature Strategy
Getting featured in TechCrunch is just the beginning. Once your article is live, make sure you maximize its impact:
-
Share it on social media channels to increase reach
-
Highlight it on your website to build credibility
-
Include it in investor pitches to showcase traction
This approach ensures that the attention you gain converts into tangible benefits for your startup.
Conclusion
Getting media coverage in a prestigious platform like TechCrunch requires preparation, storytelling, and strategic pitching. By understanding what journalists look for, building relationships, and crafting a unique narrative, you significantly increase your chances to get featured in TechCrunch.
Remember, media coverage is not just about vanity; it’s about building trust, attracting customers, and accelerating growth. Start preparing today, and your startup could be the next big story on TechCrunch.
Health
Get Featured in The Guardian: A Complete Guide to Earning Global Media Coverage
Published
1 week agoon
February 16, 2026
In today’s competitive media landscape, brands, founders, and public figures are constantly searching for credible exposure. One of the most powerful ways to build authority is to Get Featured in The Guardian — a globally respected publication known for its in-depth journalism, cultural influence, and international readership.
Being featured in The Guardian is more than just press coverage. It’s a reputation milestone. With millions of readers across the UK, US, Australia, and beyond, The Guardian has the power to amplify your story on a global scale.
This guide explains how to position your brand for success and increase your chances of securing meaningful media coverage.
Why Getting Featured in The Guardian Matters



1. Global Credibility
The Guardian is known for investigative journalism, cultural commentary, business reporting, and social impact stories. A feature instantly elevates your brand’s trust factor.
2. Massive International Reach
With a strong digital presence and global audience, your story isn’t limited to one country — it reaches readers worldwide.
3. Long-Term Brand Authority
Media coverage in a respected publication builds SEO strength, improves online reputation, and enhances investor and customer confidence.
What Type of Stories Does The Guardian Publish?
Before pitching, it’s important to understand what fits their editorial style.
The Guardian typically covers:
-
Social impact and sustainability initiatives
-
Business innovation and startup stories
-
Technology and digital transformation
-
Culture, lifestyle, and arts
-
Politics and global affairs
-
Human-interest stories with meaningful impact
They prioritize substance over self-promotion. If your story is purely promotional, it likely won’t get traction. Instead, focus on insight, originality, and relevance.
Step-by-Step Guide to Get Featured in The Guardian
1. Craft a Newsworthy Angle
Ask yourself:
-
Is this story timely?
-
Does it connect to a larger social or industry trend?
-
Does it provide new data, research, or expert insight?
Journalists look for stories that inform, educate, or challenge perspectives — not advertisements.
2. Research the Right Journalist


Don’t send generic emails. Study:
-
Which journalist covers your industry?
-
What tone do they use?
-
What topics have they recently written about?
Personalized pitches dramatically increase response rates.
3. Write a Strong Media Pitch
Your pitch should be:
-
Concise (150–250 words)
-
Clear about why the story matters now
-
Focused on value for readers
-
Free of marketing fluff
Structure:
-
Compelling subject line
-
One strong hook sentence
-
Key facts or data
-
Offer for interview or additional insights
4. Provide Supporting Materials
Make it easy for journalists:
-
High-resolution images
-
Founder bio or expert profile
-
Data reports or research findings
-
Customer case studies
-
Clear contact information
The easier you make their job, the more likely your story will move forward.
5. Work With a Strategic PR Team
Getting featured in a publication like The Guardian often requires:
-
Established media relationships
-
Deep editorial understanding
-
Strong storytelling skills
-
Timing and persistence
A professional PR strategy ensures your pitch aligns with editorial expectations and current news cycles.
Common Mistakes to Avoid
-
Sending mass, copy-paste emails
-
Pitching without understanding editorial focus
-
Making it overly promotional
-
Ignoring current news relevance
-
Following up too aggressively
Remember: journalists receive hundreds of pitches daily. Respect and relevance make the difference.
Alternative Ways to Appear in The Guardian
Getting featured doesn’t always mean a full profile story. Other opportunities include:
-
Expert commentary in industry articles
-
Op-ed contributions
-
Sponsored content (clearly labeled)
-
Data citations in investigative reports
-
Interviews as a thought leader
Each type of coverage contributes to credibility and visibility.
How Long Does It Take to Get Featured?
There’s no fixed timeline. Media placements depend on:
-
Editorial calendar
-
Current news trends
-
Story strength
-
Journalist availability
Some stories gain traction within weeks. Others require consistent outreach over several months.
Final Thoughts: Positioning Your Brand for High-Impact Coverage
To Get Featured in The Guardian, you need more than a good story — you need the right positioning, timing, and strategic outreach.
Focus on:
-
Authentic storytelling
-
Clear value for readers
-
Data-driven insights
-
Professional media communication
-
Long-term relationship building
When done correctly, a feature in The Guardian can transform your brand perception, increase digital authority, and open doors to new partnerships and opportunities.
Health
Get Featured in Marie Claire: A Complete Guide to Elevating Your Brand
Published
2 weeks agoon
February 11, 2026
Marie Claire is one of the world’s leading fashion and lifestyle magazines, known for its trendsetting content, celebrity features, and expert insights into beauty, wellness, and culture. Being featured in Marie Claire can significantly boost your brand’s credibility, enhance visibility, and open doors to a highly engaged, global audience. Whether you are a fashion designer, beauty brand, wellness expert, or entrepreneur, getting featured in this prestigious publication can be a game-changer for your business.
In this blog, we’ll explore actionable strategies, insider tips, and proven methods to help you get featured in Marie Claire and make a lasting impression.
Why Being Featured in Marie Claire Matters
-
Massive Reach and Influence
Marie Claire has a global readership across print and digital platforms. A feature in this magazine exposes your brand to millions of readers who are trend-savvy, affluent, and actively seeking innovative products and ideas. -
Credibility and Authority
Appearing in a renowned magazine instantly establishes authority. Consumers and potential collaborators perceive your brand as trustworthy and high-quality, which can increase sales, partnerships, and brand loyalty. -
SEO and Online Visibility
Digital features often include backlinks to your website, social media pages, or online store, improving your search engine ranking and online visibility. This can attract more organic traffic to your business. -
Networking Opportunities
Being featured can also catch the eye of other influencers, editors, or brands in your industry, opening doors to collaborations, interviews, and joint marketing campaigns.
How to Prepare Your Brand for a Marie Claire Feature
Before reaching out to editors, it’s crucial to ensure your brand is ready for a high-profile feature.
-
Polish Your Story
Marie Claire loves compelling stories. Whether it’s the inspiration behind your fashion line, a breakthrough in wellness, or a unique entrepreneurial journey, your narrative should be authentic, engaging, and newsworthy. -
Professional Media Kit
A media kit is your brand’s visual and informational portfolio. Include high-resolution images, product descriptions, press mentions, social media statistics, and a concise brand bio. This makes it easier for editors to understand your brand at a glance. -
Strong Online Presence
Ensure your website and social media profiles are polished and up-to-date. Marie Claire editors often check your online presence before featuring you. High-quality visuals, cohesive branding, and active engagement can make a significant difference. -
Target the Right Editor
Identify editors or writers who cover topics relevant to your brand. Marie Claire has different sections for fashion, beauty, lifestyle, wellness, and culture. A well-targeted pitch increases your chances of getting noticed.
Strategies to Get Featured in Marie Claire
1. Craft a Personalized Pitch
Generic emails rarely get noticed. Address the editor by name and explain why your story aligns with Marie Claire’s audience. Highlight what makes your brand unique and why it would appeal to their readers. Keep your pitch concise, professional, and engaging.
2. Leverage Press Agencies and PR Firms
Working with a reputable PR agency experienced in lifestyle and fashion publications can streamline the process. PR professionals have established relationships with editors and know how to craft pitches that capture attention.
3. Create Newsworthy Angles
Editors look for stories that are timely and relevant. Launching a new product, celebrating a milestone, participating in social initiatives, or introducing an innovative concept can create newsworthy angles that are more likely to be featured.
4. Utilize Influencer Collaborations
Marie Claire often covers influencers and personalities who are shaping trends. Collaborating with recognized influencers in your niche can increase your visibility and make your brand more appealing to editors.
5. Engage with the Magazine
Follow Marie Claire on social media, comment on their posts, and share content that resonates with their brand. Engaging thoughtfully can help editors recognize your brand and make future outreach more effective.
Common Mistakes to Avoid
-
Sending Mass Pitches: Editors value personalization and research. Avoid generic emails.
-
Overhyping Your Brand: While confidence is key, exaggeration can undermine credibility.
-
Ignoring Deadlines: If the magazine has submission timelines or seasonal features, missing them reduces your chances of getting featured.
-
Neglecting Visuals: High-quality visuals are critical, especially for fashion and beauty brands. Poor imagery can make your pitch less compelling.
Success Stories
Many brands and entrepreneurs have leveraged Marie Claire features to elevate their presence. For instance, indie fashion designers often see a surge in sales after a feature, while wellness brands gain recognition among a wider, lifestyle-focused audience. The exposure also leads to further media coverage, amplifying the impact.
Conclusion
Getting featured in Marie Claire is not just about prestige—it’s a strategic opportunity to grow your brand, reach a global audience, and build credibility. By crafting a compelling story, preparing a professional media kit, targeting the right editor, and leveraging PR strategies, you can increase your chances of being noticed by one of the world’s top lifestyle publications.
Whether you are launching a new product, seeking to expand your audience, or aiming to build authority in your niche, a feature in Marie Claire can be a powerful step toward achieving your business goals. Start preparing your pitch today and take the first step toward media recognition that can transform your brand.
Health
Get Published in Robb Report: The Ultimate Guide to Luxury Media Coverage
Published
2 weeks agoon
February 10, 2026
Getting featured in Robb Report is a dream for luxury brands, entrepreneurs, designers, and innovators across the world. Known as the “Voice of Luxury,” Robb Report sets the gold standard for premium lifestyle journalism, covering everything from high-end fashion and watches to real estate, yachts, travel, and elite business ventures. If you’re looking to elevate your brand’s prestige and credibility, learning how to get published in Robb Report is a powerful first step.
In this guide, we’ll walk you through why Robb Report matters, what editors look for, and how you can successfully secure a feature.
Why Getting Published in Robb Report Matters
A feature in Robb Report does more than just showcase your brand—it positions you among the world’s elite. This publication reaches affluent readers, high-net-worth individuals, luxury investors, and tastemakers who actively seek premium products and experiences.
Benefits of being featured in Robb Report include:
-
Global brand recognition
-
High-end audience exposure
-
Increased credibility and authority
-
Boost in sales and investor interest
-
Long-term reputation enhancement
For luxury brands, being published in Robb Report is not just publicity—it’s a powerful endorsement.
What Robb Report Looks For
To get published in Robb Report, your story must align with the magazine’s luxury-focused editorial standards. Editors are drawn to brands that offer:
-
Exclusivity – Limited editions, bespoke services, or one-of-a-kind offerings
-
Innovation – New technologies, unique craftsmanship, or industry-first achievements
-
Heritage & Storytelling – Rich brand history or a compelling founder journey
-
Quality & Craftsmanship – Superior materials, attention to detail, and premium positioning
-
Market Relevance – Timely stories that reflect trends in luxury, wealth, or lifestyle
Your pitch should clearly demonstrate how your brand embodies these qualities.
How to Get Published in Robb Report: Step-by-Step Guide
1. Craft a Compelling Brand Story
Your story should go beyond product features. Highlight your brand mission, founder vision, craftsmanship process, and what makes your offering exceptional in the luxury market.
2. Identify the Right Section
Robb Report covers categories such as:
-
Luxury travel
-
Real estate
-
Watches and jewelry
-
Fashion and accessories
-
Automotive and yachts
-
Fine dining and spirits
-
Business and entrepreneurship
Targeting the correct editorial section improves your chances of success.
3. Create a Media-Ready Pitch
A strong pitch should be concise, informative, and newsworthy. Include:
-
A clear headline
-
A compelling angle
-
Key brand highlights
-
Relevant data or milestones
-
High-quality visuals
-
Contact information
Avoid overly promotional language—focus on storytelling and value.
4. Leverage Professional PR Support
Working with a PR agency experienced in luxury media placements significantly increases your chances of getting published in Robb Report. Established agencies have direct media contacts, understand editorial preferences, and know how to present your story in a way that editors appreciate.
5. Follow Up Professionally
If you don’t receive an immediate response, follow up politely after 5–7 days. Persistence is important, but always remain respectful of editorial timelines.
Common Mistakes to Avoid
Many brands fail to get featured because they:
-
Send generic, mass pitches
-
Focus only on sales instead of storytelling
-
Lack professional imagery
-
Miss relevant news angles
-
Target the wrong editor or section
Avoiding these mistakes can significantly improve your success rate.
Who Can Benefit from Being Published in Robb Report?
If you fall into any of the following categories, Robb Report coverage can be especially impactful:
-
Luxury brand owners
-
High-end designers
-
Real estate developers
-
Hoteliers and restaurateurs
-
Watchmakers and jewelers
-
Tech innovators serving affluent markets
-
Entrepreneurs in premium industries
Whether you’re launching a new luxury product or expanding globally, Robb Report exposure can accelerate your growth.
How Long Does It Take to Get Published?
The timeline varies depending on your story, timing, and editorial calendar. Some features appear within weeks, while others may take several months. Seasonal trends, product launches, and major industry events often influence coverage schedules.
Why Choose Professional Help to Get Published in Robb Report?
Navigating luxury media requires expertise, relationships, and strategic storytelling. A specialized PR agency ensures:
-
Your pitch aligns with editorial standards
-
Your brand is positioned at a premium level
-
Your story reaches the right editors
-
Your campaign maximizes ROI
Professional PR support transforms your brand from being just another pitch into a compelling luxury story worthy of Robb Report’s audience.
Final Thoughts: Is Robb Report Worth It?
Absolutely. Getting published in Robb Report is one of the most effective ways to elevate your brand’s image, authority, and influence within the luxury market. The credibility that comes with this feature cannot be replicated through traditional advertising.
If your brand represents excellence, exclusivity, and innovation, Robb Report is the platform that can showcase your story to the world’s most discerning audience.
Looking to get published in Robb Report? Partner with a trusted PR agency that understands luxury storytelling and media placement to secure your feature and elevate your brand’s global presence.
Health
Get Published In Glamour Magazine: A Complete Guide for Brands, Creators, and Entrepreneurs
Published
2 weeks agoon
February 9, 2026
Getting featured in Glamour Magazine is a dream for many brands, entrepreneurs, and creatives—and for good reason. Glamour is one of the world’s most influential lifestyle and fashion publications, known for spotlighting inspiring stories, trendsetting products, and powerful voices. If you’re looking to get published in Glamour Magazine, this guide will walk you through everything you need to know to increase your chances of success.
Why Getting Published in Glamour Matters
Glamour reaches millions of readers globally across print, digital, and social platforms. A feature in Glamour can:
-
Build instant brand credibility
-
Boost online visibility and traffic
-
Attract investors, partners, and customers
-
Position you as a thought leader in your industry
Whether you’re a startup founder, fashion brand, beauty entrepreneur, wellness expert, or influencer, a Glamour feature can elevate your brand to the next level.
What Kind of Stories Does Glamour Publish?
To get published in Glamour Magazine, your story must align with their editorial focus. Glamour typically features:
-
Women-led businesses and entrepreneurs
-
Fashion, beauty, wellness, and lifestyle brands
-
Social impact stories and empowerment narratives
-
Cultural trends and innovation
-
Personal journeys that inspire or educate
Before pitching, study recent Glamour articles to understand tone, themes, and style.
How to Get Published in Glamour Magazine
1. Craft a Compelling Story Angle
Journalists aren’t looking for advertisements—they want stories. Ask yourself:
-
What makes your brand or journey unique?
-
What problem are you solving?
-
Why should readers care?
Your pitch should focus on value, relevance, and impact, not promotion.
2. Identify the Right Editor or Section
Glamour has different editors for fashion, beauty, culture, wellness, business, and more. Pitching the right person increases your chances significantly.
3. Write a Strong Media Pitch
Your email pitch should be:
-
Short and personalized
-
Clearly state why your story fits Glamour
-
Include a compelling subject line
-
Offer exclusive insights or expert commentary
Example subject line:
Story Pitch: Female Founder Revolutionizing Clean Beauty
4. Build Your Media Presence
Having an active online presence helps journalists trust your credibility. Make sure your website, social media, and past media mentions are professional and updated.
5. Work with a Professional PR Agency
Getting published in top-tier media like Glamour is highly competitive. A PR agency with strong editorial connections can:
-
Pitch your story strategically
-
Position your brand effectively
-
Handle follow-ups and negotiations
-
Increase acceptance rates
Common Mistakes to Avoid
-
Sending mass, generic pitches
-
Making the pitch overly promotional
-
Ignoring Glamour’s editorial guidelines
-
Failing to follow up professionally
-
Pitching irrelevant topics
Avoid these mistakes to improve your chances of getting published.
How Level Up PR Helps You Get Published in Glamour Magazine
At Level Up PR, we specialize in securing high-impact media placements in top-tier publications, including Glamour Magazine. Our expert PR strategists:
-
Develop powerful brand narratives
-
Identify the best editorial opportunities
-
Pitch directly to relevant Glamour editors
-
Position you as a trusted expert or trendsetter
With our proven media relationships and storytelling expertise, we help brands turn visibility into long-term growth.
Final Thoughts
Getting published in Glamour Magazine is not just about publicity—it’s about credibility, influence, and growth. With the right story, strategy, and media connections, your brand can earn its place in one of the world’s most respected publications.
If you’re ready to get published in Glamour Magazine, now is the time to take action and elevate your brand’s story.
Health
Get Published in Wall Street Journal: A Complete Guide for Brands and Entrepreneurs
Published
3 weeks agoon
February 6, 2026
Getting published in The Wall Street Journal (WSJ) is a powerful credibility booster for any brand, entrepreneur, or industry leader. As one of the most respected and widely read business publications in the world, a feature in WSJ can significantly enhance your reputation, attract investors, build trust with customers, and elevate your market presence. But how exactly do you get published in the Wall Street Journal? This guide breaks down the process and provides practical tips to improve your chances of success.
Why Getting Published in the Wall Street Journal Matters
The Wall Street Journal reaches millions of readers globally, including business executives, policymakers, investors, and decision-makers. A feature in WSJ does more than generate exposure—it positions you as a credible authority in your industry. Whether you’re launching a startup, scaling a company, or establishing thought leadership, WSJ coverage can:
-
Build instant trust and brand authority
-
Increase website traffic and lead generation
-
Attract partnerships and investment opportunities
-
Strengthen your PR and marketing strategy
Because of its prestige, WSJ is highly selective about what it publishes, making preparation and strategy essential.
Understand What WSJ Journalists Look For
Before pitching, it’s important to understand the type of stories WSJ prefers. They focus on business, finance, economics, technology, markets, leadership, entrepreneurship, and global affairs. Journalists look for stories that are:
-
Timely – Related to current events, trends, or market changes
-
Newsworthy – Offering new insights, data, or developments
-
Impactful – Relevant to a broad business or consumer audience
-
Credible – Backed by facts, data, and reliable sources
Promotional content or sales-focused pitches are unlikely to succeed. Instead, your story should provide value to readers.
Identify the Right Angle for Your Story
To get published in Wall Street Journal, your story must go beyond your brand and focus on a broader narrative. Ask yourself:
-
Does this story reflect a larger industry trend?
-
Can it offer expert insight into a current business challenge?
-
Does it provide data, research, or analysis that adds value?
For example, instead of pitching “Our company launched a new product,” consider framing it as “How emerging startups are transforming [industry] through innovation,” with your brand as a real-world example.
Research the Right Journalist or Editor
WSJ has dedicated journalists covering specific beats such as technology, startups, finance, real estate, health, and global markets. Study recent articles in your industry and identify reporters who consistently cover similar topics.
When you find the right journalist:
-
Read their work to understand their tone and interests
-
Personalize your pitch to match their beat
-
Reference one of their recent articles to show relevance
A targeted pitch is far more effective than sending a generic email to a newsroom.
Craft a Compelling Pitch
Your pitch should be concise, informative, and news-driven. Aim for 3–5 short paragraphs that clearly explain:
-
Your story angle – What’s the news or insight?
-
Why it matters – How does it impact businesses, markets, or consumers?
-
Why now – Why is this story timely?
-
Your credibility – Why you’re a reliable source on this topic
Avoid exaggerated claims or promotional language. Keep the focus on the story, not on selling your product or service.
Provide Supporting Data and Sources
WSJ values accuracy and depth. Strengthen your pitch by including:
-
Market data or industry statistics
-
Results from surveys or original research
-
Case studies or real-world examples
-
Quotes or insights from credible experts
Providing reliable information increases your chances of being taken seriously and may even shape the angle of the final article.
Prepare for Media Interviews
If a journalist shows interest, be ready for an interview. Preparation is key. Ensure you can:
-
Clearly explain your insights in simple, non-technical language
-
Share real examples, numbers, or outcomes
-
Stay on message while answering questions honestly
Remember, journalists are looking for value for their readers—not promotional soundbites.
Consider Guest Opinion or Thought Leadership Pieces
In addition to news features, WSJ sometimes publishes opinion pieces, expert columns, and thought leadership articles. These pieces typically focus on industry analysis, economic trends, leadership insights, or policy commentary.
To succeed with an opinion submission:
-
Present a strong, original viewpoint
-
Support your argument with data and logic
-
Keep the tone authoritative, informative, and professional
This route is especially effective for executives, founders, and industry experts looking to build authority.
Leverage Professional PR Support
Getting published in the Wall Street Journal is highly competitive. Many businesses choose to work with experienced PR agencies that have established media relationships, pitching expertise, and a deep understanding of editorial standards. A professional PR team can:
-
Refine your story angle
-
Identify the right journalists
-
Craft compelling pitches
-
Manage media outreach and follow-ups
This strategic support can significantly improve your chances of earning top-tier media coverage.
Final Thoughts
Getting published in Wall Street Journal is not about luck—it’s about strategy, storytelling, and credibility. By understanding what journalists look for, crafting a strong narrative, providing valuable insights, and approaching the right reporters, you can position yourself for meaningful media exposure.
Whether you’re a startup founder, business leader, or growing brand, WSJ coverage can be a powerful asset in building trust, authority, and long-term success. With the right approach, your story can earn a place in one of the world’s most influential publications.
Trending
-

 Health5 years ago
Health5 years agoEva Savagiou Finally Breaks Her Silence About Online Bullying On TikTok
-

 Health4 years ago
Health4 years agoTraumatone Returns With A New EP – Hereafter
-

 Health4 years ago
Health4 years agoTop 5 Influencers Accounts To Watch In 2022
-

 Fashion5 years ago
Fashion5 years agoThe Tattoo Heretic: Kirby van Beek’s Idea Of Shadow And Bone
-

 Fashion4 years ago
Fashion4 years agoNatalie Schramboeck – Influencing People Through A Cultural Touch
-

 Fashion9 years ago
Fashion9 years ago9 Celebrities who have spoken out about being photoshopped
-

 Health5 years ago
Health5 years agoBrooke Casey Inspiring People Through Her Message With Music
-

 Health5 years ago
Health5 years agoTop 12 Rising Artists To Watch In 2021
-

 Health5 years ago
Health5 years agoMadison Morton Is Swooning The World Through Her Soul-stirring Music
-
 Health4 years ago
Health4 years agoTop 10 Influencers To Follow This 2021