A worrying health trend is quietly unfolding across the United States. According to a new study by the Centers for Disease Control and Prevention (CDC), invasive group A streptococcus infections — a severe form of the common strep bacteria — have more than doubled over the past decade. The findings, published in the Journal of the American Medical Association, shed light on a once-stable disease that is now rapidly gaining momentum and becoming a serious public health concern.
From Common Germ to Killer Infection
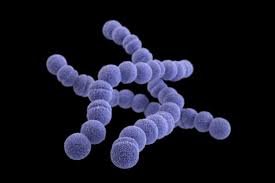
Group A streptococcus is the same bacteria responsible for strep throat — a typically mild illness. But in its invasive form, the pathogen turns deadly, capable of triggering necrotizing fasciitis (flesh-eating disease) and streptococcal toxic shock syndrome, which can lead to multiple organ failure. In these cases, the bacteria penetrate parts of the body normally free from germs, like the bloodstream, lungs, or deep muscle tissue.
“Within 24 to 48 hours, you could have very, very rapid deterioration,” said Dr. Victor Nizet, professor of pediatrics at the University of California, San Diego. “Cases can go from seeming like a routine flu-like illness to rushing the patient to the ICU, fearing for their recovery.”
The numbers are stark. In 2013, the rate of invasive strep was roughly 4 per 100,000 people. By 2022, it had climbed to 8 per 100,000. Across 10 states studied — representing 35 million people — cases jumped from just over 1,000 to nearly 2,800 annually. Over the nine-year span, more than 21,000 cases were recorded, with almost 2,000 deaths. Extrapolated nationwide, experts believe the real death toll could exceed 10,000.
“This data is a red flag,” said Dr. Christopher Gregory, a CDC researcher and one of the study’s authors. “The threat of invasive strep has substantially increased, especially for high-risk populations.”
Who’s at Risk?
The study found that the highest rates of infection occurred in adults over the age of 65, but the trend was upward across all adult age groups. Surprisingly, the data did not reflect a similar rise in children. However, pediatric specialists say that doesn’t match what they’re seeing on the ground.
“That was, to me, the most shocking part of the study,” said Dr. Allison Eckard, division chief for pediatric infectious diseases at the Medical University of South Carolina. “Clinically, we are seeing what feels like an increase — and not just more cases, but more severe ones.”
She pointed to an alarming spike in pediatric cases in late 2022, which prompted a CDC alert. Hospitals reported children presenting with rare and aggressive forms of the infection, including necrotizing fasciitis. These cases were often associated with other respiratory illnesses like influenza, RSV, or COVID-19, which may weaken the immune system and allow invasive strep to take hold.
“We’re seeing more unusual cases, and that raises concern that there is something going on more nationally,” Eckard added.

A Silent Surge: Invasive Strep Infections Double Across
What’s Driving the Surge?
Several factors appear to be fueling this sudden rise. First, underlying health conditions like diabetes and obesity — both of which are on the rise in the U.S.—can compromise the immune system and make people more vulnerable. These conditions also increase the likelihood of skin infections, which can be an entry point for the bacteria.
Another key factor is the increase in infections among people who inject drugs or are experiencing homelessness. In 2022, the rate of invasive strep among the homeless population was a staggering 807 per 100,000 — one of the highest infection rates ever documented globally. Open wounds, limited access to hygiene, and crowded living conditions all contribute to this vulnerability.
Moreover, the bacteria itself is changing. The study found that newer strains of group A strep are more likely to cause skin infections than throat infections and are becoming more genetically diverse. Some of these strains are also showing resistance to commonly used antibiotics like macrolides and clindamycin, which are sometimes used in cases where penicillin — the standard treatment — isn’t suitable.
A Call for Urgent Action
With antibiotic resistance growing and infections surging, experts say the time has come to seriously consider a vaccine for group A strep. However, vaccine development has faced major hurdles.
“The lack of a vaccine is devastating,” said Dr. Nizet. “There’s growing concern about recent shifts in attitudes at the FDA and CDC, which seem to be slowing down progress in vaccine development.”
Accelerated research, broader surveillance, and improved access to care for vulnerable populations are all being called for in response to the study’s findings. Doctors emphasize the importance of recognizing symptoms early. Warning signs of invasive strep include severe pain, fever, swelling, and rapidly worsening flu-like symptoms. If caught early, treatment with antibiotics can be effective — but time is critical.
Public health officials are also encouraging hospitals and clinicians to report cases and track bacterial strains more closely. “This is a critical moment to reassess how we monitor, prevent, and respond to invasive strep,” said Gregory.
As the U.S. healthcare system continues to grapple with the aftermath of the COVID-19 pandemic, the rise in invasive group A strep infection serves as a stark reminder of the need for vigilance. A familiar bacteria has taken a dangerous turn, and experts warn that without targeted intervention, the trend could get worse.
Whether through improved healthcare access, public education, or renewed focus on vaccine development, one thing is clear: the fight against invasive strep can no longer be overlooked.